- Jose Luis Dieppa
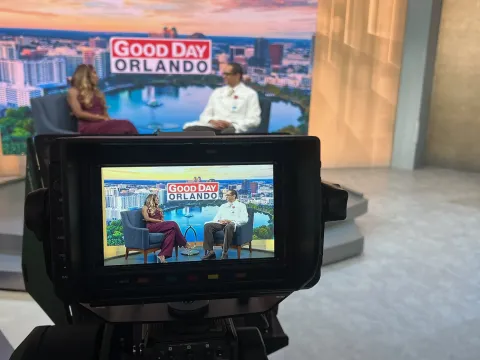
Deep Brain Stimulation - AdventHealth TV Story
At just 35 years old, Carlos Paredes got a stunning diagnosis: He had Parkinson’s disease.
“I did not want to believe that I had Parkinson’s at my age,” he said. “At that time, I was about to get married, and I was ready to start a family. So, it was hard for me.”
Paredes initially noticed tremors in one of his fingers. Over the years the uncontrollable movements spread to all his fingers, and eventually to both arms. The tremors were so severe that he struggled with simple tasks such as drinking from a cup, writing and brushing his teeth.
“My movements increased to the point I could not hold a plate for dinner, I could not play with my daughter or shave,” he said.

His family advised him to see a neurologist, who diagnosed him with Parkinson’s disease – a progressive condition that causes tremors, slowness and balance issues. After years of taking up to 16 pills daily without much improvement, his mother suggested he see an expert in brain surgery.
In consultation with his medical team, which included neurosurgeon Dr. Chandan Reddy at AdventHealth Celebration and Dr. Mitesh Lotia, movement disorder neurologist and medical director of the movement disorder program at AdventHealth, it was determined that Paredes was an ideal candidate for deep brain stimulation surgery.
“Deep brain stimulation is a procedure where we insert two small wires into either side of the brain. They stimulate a very specific area of the brain to help treat tremors and other symptoms of Parkinson’s disease,” said Dr. Lotia.
By implanting electrodes, doctors can stimulate the specific areas of the brain associated with the unique condition of the patient through electrical impulses that regulate signals, cells and chemicals. A pacemaker-like device is implanted under the skin of the patient’s chest that controls the amount of stimulation the patient receives, and a wire connects the device to the electrodes in the brain. After surgery, visits are frequent in the first several months for therapy management and require in-person visits to ensure the device is working properly and to modify settings when needed.
But thanks to innovative new technology, the adjustments can now be done remotely through the NeuroSphere Virtual Clinic. The process is simple. Using a tablet, Dr. Lotia can observe Paredes’ symptoms and change the stimulation in his brain during a telehealth visit, which can be done from anywhere, such as the patient’s home or workplace. The results can be seen immediately.
“Doing this virtually pretty much serves the same purpose of doing it in clinic,” said Dr. Lotia. “We can provide the same and effective care in the comfort of their home or, as in Carlos’ case, their work.”
"My life has improved 90% because I do not have the movements anymore."
Deep brain stimulation surgery can improve the quality of life of the patient, including returning to hobbies, sports, and other activities. It can also help the patient manage their symptoms as the disease changes or progresses.
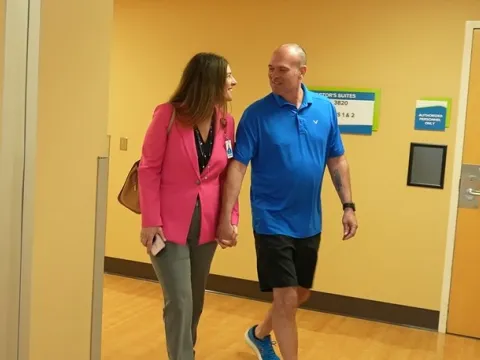
For Paredes, the procedure permitted him to return to the things he loves, including his job.
“My life has improved 90% because I do not have the movements anymore. I can play with my daughter, I can do my job normally, I can have a life with my family,” he said.
According to Dr. Lotia, about 15% of patients with Parkinson’s disease in the United States become good candidates for deep brain stimulation surgery. However, it is still a very underutilized service due to many factors such as lack of awareness, delayed referrals and fear of brain surgery.
“I was very scared of the procedure, but I did it for family,” Paredes said. “I hope that people who may have the same condition see my story and get the help they need. If I can help one person, it was all worth it.”
To hear more about Paredes’ journey, watch the video that originally appeared on “AdventHealth TV,” AdventHealth’s internal newscast for Central Florida Division team members.
Recent News

Expanding hope through innovation: AdventHealth advances cancer care across East Florida
Cancer touches nearly every family, and in Flagler, Lake and Volusia counties, the demand for timely, advanced care keeps rising. AdventHealth’s East Florida Division, which includes seven hospitals...
New surgeon expands local access to advanced colorectal care in Volusia County
Dr. Mark Heimberger joins AdventHealth as part of its continued investment in bringing minimally invasive and robotic colorectal treatment options to the region’s growing community.
Robotic surgery in the spotlight
Dr. Abubaker Ali joined FOX 35’s HouseCalls to share how robotic surgery is transforming care for patients across Flagler, Volusia and Lake counties. He highlighted how this technology supports...

A new option for hope: Daytona Beach team performs groundbreaking heart procedure
Innovative technique expands life-saving options for patients once considered inoperable.

Easing the winter blues: Experts share how to restore wholeness to body, mind and spirit
Connection, movement, light therapy and mindful care can help lift your mood and bring balance back during the darker winter months.

Three local women honored for turning cancer journeys into community healing
The AdventHealth Palm Coast Foundation has named Carla Cline, Nancy Katz-Arceo and Muffy Runnells its 2025 Humanitarians of the Year.

New heart procedure helps Lake County residents lower stroke risk
Minimally invasive WATCHMAN FLX Pro procedure offers patients a safer, local option for stroke prevention.

How one caregiver’s simple coin for veterans became a symbol of healing
At AdventHealth Waterman, the small gift honors veterans year-round and turns care into tribute, inviting stories to surface.

Q&A: How AdventHealth is redefining nurse growth through whole-person care
AdventHealth’s model for nursing career growth prioritizes nurses’ whole health to support their care for the body, mind and spirit.

From Matanzas High School to modern medicine
When Bianca Iglesias decided to become a nurse practitioner, her goal was simple: to care for people the way she saw her grandfather cared for during his final days.

Doctors agree: There's no quick fix for a cold, but these tips can make it more bearable
Waking up with a cold isn’t anyone’s idea of a good time.
Routine test leads Palm Coast man to lifesaving robotic surgery
What started as a routine at-home screening turned into a life-changing experience for Doug Fritz of Palm Coast, one that reminded him of the power of modern medicine and the compassion behind it.
