
A Community of Physicians for Better Health Care
Adventhealth Provider Network (AHPN) is a like-minded community of providers collaborating at the highest level to transform how health care is delivered.
Our network of employed and independent providers receive administrative support that enhances the quality of care and improves the patient experience, all while reducing cost. Providers also receives health management services for high-risk patients, actionable data and a performance and enablement team to help them navigate the population health journey.
Network Benefits for
Primary Care Providers
AdventHealth Provider Network's (AHPN) success relies on a foundation of primary care providers (PCPs) who excel in delivering value-based care across their communities. PCPs participating in AHPN prioritize creating access and providing a holistic approach to patient care by closing care gaps, ensuring proper coding and documentation are used, and engaging in thoughtful referral management. A primary objective of AHPN is the success of our participating providers. Our network performs at the highest levels and sustains this success by supporting our PCPs to maintain engagement and performance service standards.
High-performing PCPs are eligible to participate in the Performance Incentive Program. This initiative encourages, identifies and rewards top performers in cost, utilization, quality, access to care, and coding and documentation integrity in the network. Our PCPs also have access to the exclusive benefits detailed below.
The opportunity to participate in AHPN's diverse payor and direct-to-employer contracts. AHPN supports increased patient access, growing panels and patient care by:
- Enhanced patient services: Specialized services, including chronic care management, emergency department care coordination and transitional care management, support practices in delivering comprehensive and continuous patient care.
- Prioritized patient reporting: Network participants receive streamlined and prioritized reports tailored to improve efficiency and quality.
- Focus on patient care: With our support in clinical documentation and operational management, PCPs can concentrate on what matters most — patient care.
PCPs who lower health care expenditures, raise quality outcomes and improve patient experience participate in AHPN’s pay-for-performance and shared savings arrangements that are part of our value-based contracts.
- Quarterly incentive revenue: By achieving targets for key performance metrics in cost of care, utilization, quality, access to care and clinical documentation integrity, PCPs can earn quarterly incentives.
- Annual shared savings: When AHPN achieves its goals, PCPs receive annual shared savings (proportional to the practice’s membership share) and share in the collective success of our network
AHPN is physician-led, which gives physicians a voice in contract quality measures, payment structure and network oversight.
- Collaborative community: Our PCPs are a network of peers dedicated to advancing value-based health care. Our structure is designed to promote collaborative learning and the sharing of insights to collectively shape a better future for health care.
Network PCPs benefit from a dedicated support team that provides them with the tools and resources for continued success in managing the care of their patients.
- Regular performance reporting: PCPs stay informed with insights that help track their performance progress and identify areas for improvement through monthly/quarterly meetings and reports.
- Streamlined performance program: PCPs receive support to help them navigate the complexities of disparate payor programs with ease. AHPN's cohesive performance program harmonizes various requirements, simplifying PCP participation and maximizing network benefits.

Network Benefits for Specialty Physicians
We are an network that includes specialists who are highly aligned to the Clinically Integrated Network (CIN) and are expected to achieve performance goals. Some of the benefits to specialists within our network are:
- Increased patient access due to participation in exclusive contracts only available to CIN-affiliated physicians
- Competitive fee schedules
- AHPN specialists remain the preferred referral source for Network PCPs.
How We're Building Value
With a focus on value, AHPN brings patients, payors, physicians, facilities and other health care services together into contractual relationships that benefit all parties.
- Patient Value
-
- Quality care: AHPN delivers the highest quality of care by adhering to evidence-based, national best practices.
- Patient experience: Our patients feel supported during their journey within AHPN as they navigate the complexity of the health care system.
- Lower total cost of care: AHPN strives to provide affordable care through the appropriate use of health care resources and the delivery of care in the right setting.
- Value for Payors
-
- High quality at a lower total cost of care: Payers and employers are looking for lower costs and high-quality care for their members. AHPN delivers both.
- Managed network: Payers and employers want a dedicated group of providers who work together to provide excellent collaborative care by providing appropriate preventive care and integrated delivery of health care services while increasing the patient experience for their members.
- Transforming Care and Advancing Value
-
Every year, our AdventHealth Provider Network (AHPN) shares how we delivered on our promise to improve care quality, enhance the patient experience and reduce the total cost of care across Florida and beyond.
The 2024 Annual Value Report highlights our latest results and innovations — and the extraordinary partnerships powering our performance.
Who We Support
Types of contracts:
- Full risk
- Network access
- Pay-for-performance
- Shared savings: upside only
- Shared savings: upside and downside
High-Performance Provider Expectations
We have the following provider performance expectations of all participants that join AHPN.
- Invest time and resources in the patients attributed to you through our value-based contracts.
- Commit to AHPN clinical guidelines and performance-improvement activities.
- Share data to facilitate clinical integration activities.
- Identify patients needing chronic care management (CCM) programs or annual visits.
- Document all patient conditions to the highest level of specificity.
- Ensure downstream network-referral management occurs.
- Commit to allowing remote read-only access to the electronic health record (EHR).
Delivering Better Patient Experiences and Healthier Communities
AHPN is transforming how health care is delivered to the community. We are a physician-led network that enhances the quality of care and improves the patient experience while reducing costs.
AHPN brings together more than 5,700 AdventHealth employed and independent community providers, including primary care and medical/surgical specialties, who are coordinated and committed to improving the patient health care journey experience.
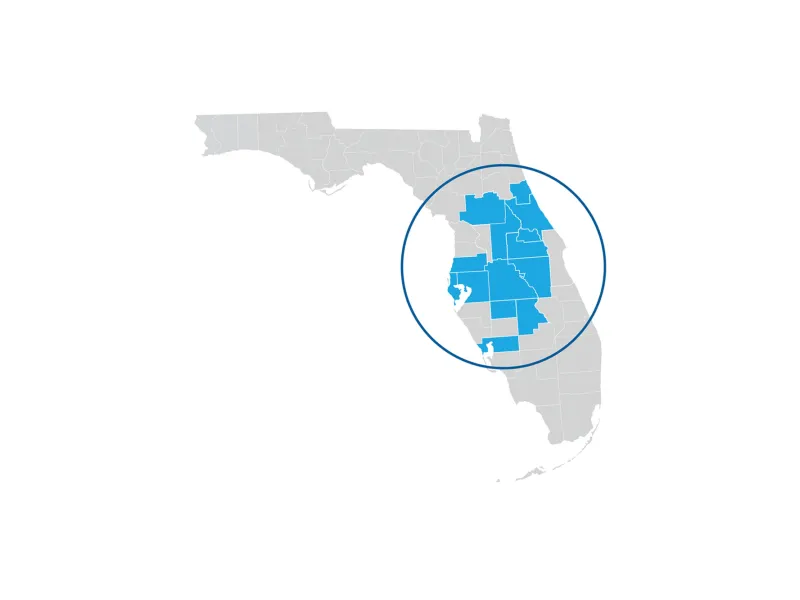
Our Florida Network
AHPN provides high-quality care and access across the state of through our comprehensive network of providers.
- Covers a 14-county market area
- More than 5,700 employed and independent providers, including primary care and most medical/surgical specialties
Clinical Care and Sites of Service include:
- Hospitals
- Ambulatory surgery centers
- Home health
- LTAC
- Urgent care
- Imaging centers
- Home infusion
- Skilled nursing facilities
- Outpatient rehabilitation
- Outpatient infusion and chemotherapy
- Hospice
A Team of Support Behind Participating Providers
- Network Management
-
The Network Management team supports network providers by verifying and updating provider information, assisting with network onboarding, contracting, credentialing and claims escalation issues. AHPN practices will have an assigned provider outreach representative, who will be the practice’s first and primary contact for support. This team also works to connect the practice with additional support teams as needed, such as the Performance and Enablement team or the Quality team.
- Provider Performance and Enablement
-
The Provider Performance and Enablement team helps AHPN providers achieve practice transformation goals and improve performance standings in the network by delivering the following services:
- Detailed attributed patient lists and performance reports
- Value-based onboarding and education
- Value-based performance questions
- Performance support tools
- Performance visits with practices
- Practice transformation
- Attribution questions
- Quality
-
The Quality team supports participating providers to ensure the delivery of high-quality care and quality metrics tied to AHPN contracts. The team identifies opportunities to improve quality and manage quality programs to support the practice and its patients.
The Quality team comprises subject-matter experts in quality metrics, chart abstraction, metric definition (including numerator and denominator) and national benchmarks.
- Clinical Documentation Integrity
-
The Clinical Documentation Integrity Coding (CDI) team supports AHPN providers with questions regarding risk adjustment. They provide education and materials on good coding and documentation practices and how hierarchical condition codes work. The team includes senior CDI specialists who will meet AHPN providers in their practices to address CDI needs.
- Care Management
-
The Care Management team is a group of highly trained registered nurses, social workers, pharmacists and whole-health coordinators. They provide a whole-person care management program that addresses high-risk and rising-risk patients' physical, mental and social needs.
The program aims to improve high-risk patients' overall health, as evidenced by lower readmission rates, improved clinical outcomes and decreased total cost of care. Care management can assist AHPN providers with patients who present the following criteria.
- One or more of these disease states when clinically assessed as poorly controlled: Asthma (pediatric or adult)
- Chronic kidney disease
- Chronic obstructive pulmonary disease
- Congestive heart failure
- Coronary artery disease
- Diabetes
- Hypertension
- Frequent avoidable utilization (such as excess use of emergency services)
- Depression screening requiring behavioral health care coordination
- Social determinants of health screening requiring assistance with connecting to community resources
- ED Care Coordination Center
-
The Emergency Department Care Coordination Center (ED CCC) provides alternatives to inpatient admission for select patients of AHPN providers in the emergency department. This team of nurses follows the network provider's patients in the ED and communicates with the ED providers to offer alternatives to inpatient admission.
Contact Us
If you are a value-base care focused provider interested in joining the network, please contact our Provider Experience Center at 877-850-5438, Monday through Friday from 8 am to 5 pm.

