- AdventHealth

The AMBASSADOR Phase III clinical trial results, recently published in the New England Journal of Medicine, revealed that adjuvant pembrolizumab (brand name Keytruda), a programmed death 1 (PD1) checkpoint inhibitor immunotherapy, significantly extended disease-free survival in patients with high-risk, muscle-invasive urothelial carcinoma after radical surgery.
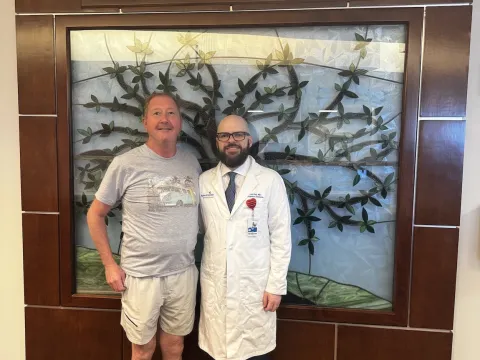
Approved by the National Cancer Institute (NCI) Cancer Therapy Evaluation Program (CTEP), this multi-center trial was conducted by the Alliance for Clinical Trials in Oncology (Alliance) and the National Clinical Trials Network (NCTN). AdventHealth Clinical Research Unit (CRU) Executive Director and Medical Director of Genitourinary Oncology Guru Sonpavde, MD, co-authored the article and served as the lead principal investigator for the Southwest Oncology Group (SWOG), part of the Alliance.
“In our study, the median disease-free survival with pembrolizumab was double that seen with observation, and it also led to an approximately 30% reduction in the risk of the cancer recurring,” shares Dr. Sonpavde. “We continue to make significant advances in immunotherapies that are helping to improve the cure rate for this highly aggressive and difficult to treat cancer.”
The Challenge of Treating Urothelial Cancer
Muscle-invasive urothelial carcinoma is an aggressive disease with high rates of relapse. In fact, about 50% of patients with the disease experience recurrence of their cancer after surgery. For many years, the standard of care was radical surgery with neoadjuvant cisplatin-based chemotherapy.
“Neoadjuvant chemotherapy has an overall survival benefit, but many patients are not eligible for this therapy or decline it,” explains Dr. Sonpavde. “Additionally, while we know adjuvant cisplatin-based chemotherapy can lengthen disease-free survival in patients who did not have chemotherapy prior to their surgery, up to one-third of patients are not medically fit to receive chemotherapy post-operatively.”
The Role of Checkpoint Inhibitors
A type of immunotherapy, checkpoint inhibitors have emerged as a new approach to treating cancer. They block specific proteins that prevent the immune system from attacking cancer cells.
In addition to the AMBASSADOR study, several other clinical trials have explored the safety and effectiveness of checkpoint inhibitors in treating patients with urothelial cancer. The CheckMate 274 trial compared adjuvant nivolumab (brand name Opdivo), another PD1 inhibitor immunotherapy, with placebo and demonstrated improvements in disease-free survival, leading to the drug’s approval by the U.S. Food and Drug Administration (FDA) in 2021. More recently, the CheckMate 901 Phase III clinical trial found that combining nivolumab with gemcitabine-cisplatin chemotherapy increased survival rates for patients with unresectable or metastatic urothelial carcinoma.
“Both nivolumab and pembrolizumab are antibodies directed against PD-1, and based on these other studies, we expected to achieve positive results with the AMBASSADOR trial,” says Dr. Sonpavde.
In this latest trial, 702 patients underwent randomization with 354 assigned to receive pembrolizumab and 348 to observation. With a median duration of 44.8 months follow-up, median disease-free survival was 29.6 months with pembrolizumab compared to 14.2 months with observation. The adverse-event profile was consistent with what had previously been reported with no new safety concerns.
“Our findings tell us we’re moving in a good direction, and we’re hopeful that our work will lead to FDA approval of adjuvant pembrolizumab for muscle-invasive urothelial carcinoma within the next 6 months,” reports Dr. Sonpavde.
Additional Research on Treating Urothelial Cancer with Checkpoint Inhibitors
Earlier this year, Dr. Sonpavde and his team at AdventHealth Cancer Institute became one of the first in the world to offer a new, global Phase II clinical trial that is evaluating the efficacy and safety of pembrolizumab plus V940 (mRNA-4157) in patients with high-risk, muscle-invasive urothelial carcinoma of the bladder and upper urinary tract following radical resection. V940 is a novel, customized immunotherapy that consists of mRNA that encodes up to 34 neoantigens (new mutated proteins) found specifically in an individual patient’s tumor. A precision immunotherapy, V940 is designed to activate the immune system to target these neoantigens.
“The V940 trial builds upon what we achieved in the AMBASSADOR trial to see if we can further enhance survival for patients suffering from this aggressive cancer,” comments Dr. Sonpavde. “With this new trial, we’re trying to improve the cure rate for these patients by killing the microscopic cancer cells that remain after surgery."
Dr. Sonpavde believes future research efforts will start to evaluate the use of these new immunotherapies earlier in the disease process. He shared that a study called NIAGARA was recently presented at the European Society of Medical Oncology meeting. It looked at another immunotherapy called durvalumab delivered neoadjuvantly in combination with chemotherapy followed by radical cystectomy and then adjuvant durvalumab in patients with muscle-invasive bladder cancer. The NIAGARA study also demonstrated meaningful improvement in overall survival.
“At AdventHealth, we’re excited about all of these advancements in the quest to cure cancer and remain committed to exploring the potential power of innovative approaches through our research efforts,” states Dr. Sonpavde. “I strongly encourage referral of patients to our many clinical trials, which provide them access to some of the latest treatment options.”
Recent News

AdventHealth Cancer Institute Advances the Use of CAR T-Cell Therapy for Multiple Myeloma
CAR-T therapies have emerged as new treatment options for certain types of cancer through a one-time infusion that can lead to long-lasting remission.

AdventHealth Graduate Medical Education Program Celebrates 50 Years
Growing from a family practice residency to 24 accredited programs, AdventHealth’s Graduate Medical Education (GME) program celebrates 50 years.

New Clinical Trial Explores Digital Intervention for Apathy in Late-life Depression
Afflicting 30-50% of patients with late-life depression, apathy is a challenging psychiatric syndrome in older adulthood that can result in lack of motivation leading to poor self-care, physical...
AdventHealth Performs Central Florida’s First Liver Transplant for Unresectable Colorectal Liver Metastases
In June 2025, AdventHealth Abdominal Transplant Surgeon and Surgical Oncologist Ryan Day, MD, worked with a multidisciplinary team to perform Central Florida’s first liver transplant for unresectable...

AdventHealth Neuroscience Institute First in Florida to be Recognized as a GammaTile Center of Excellence
GammaTile is the first and only tile-based radiation therapy for the treatment of
operable brain tumors. The AdventHealth Neuroscience Institute began performing GammaTile procedures in 2021 and was...

An AdventHealth Collaboration Explores the Impact of Microgravity and Electrical Stimulation on Muscle Cell Health in Space
Using a muscle lab-on-chip model aboard the International Space Station (ISS), AdventHealth Translational Research Institute’s Dr. Paul Coen has been working with a multidisciplinary team from the...

AdventHealth Neuroscience Institute Among First in U.S. to Offer Phase IIa Clinical Trial of Troculeucel for Moderate Alzheimer’s Disease
While most clinical trials for Alzheimer’s disease have focused on patients with early or mild cognitive impairment, roughly 30% of those with Alzheimer’s have moderate stage disease for which there...

AdventHealth Translational Research Institute Selected as Clinical Site for National Study of Muscle, Mobility and Aging (SOMMA)
Under the leadership of Scientific Director and Principal Investigator Bret H. Goodpaster, PhD, the AdventHealth Translational Research Institute (TRI) is now enrolling men and women 70 years of age...

AdventHealth Neuroscience Institute Administers First Dose of Investigative NK Cell Therapy to Person with Alzheimer’s Disease
Under a single compassionate use Investigational New Drug (IND) authorization cleared by the U.S. Food and Drug Administration (FDA), the AdventHealth Neuroscience Institute worked with NKGen Biotech...

New Study Published in the New England Journal of Medicine Shows the Addition of Regional Nodal Irradiation Does Not Decrease Rate of Invasive Breast Cancer Recurrence in Patients with Negative Axillary Nodes Following Neoadjuvant Chemotherapy
Findings of the phase III, multicenter, randomized NSABP B-51-RTOG 1304 clinical trial were recently published in the New England Journal of Medicine with AdventHealth Cancer Institute’s Dr. Mamounas...

AdventHealth Study Exploring the Use of MR-Guided Focused Ultrasound (MRgFUS) to Disrupt the Blood-Brain Barrier for Treatment of Alzheimer’s Disease
Under the leadership of Dr. Valeria Baldivieso and Dr. Chandan Reddy, the AdventHealth Research Institute is the first and only site in Orlando offering the Exablate Blood-Brain Barrier (BBB)...

AdventHealth Research Institute Offers Phase II Clinical Trial of Etanercept for Treatment of Blast-Induced Tinnitus
Approximately 1 billion people throughout the world suffer from tinnitus (ringing in the ears), and it is the number one disability of those who serve in the U.S. military. The condition can disrupt...
