- AdventHealth
After nearly 10 years as part of the TrialNet studies, physicians at AdventHealth Central Florida Division are now administering the world’s first treatment to delay the onset of Type 1 diabetes (T1D). While we always thought this disease was incurable, the treatment AdventHealth researchers helped contribute to is now approved by the U.S. Food and Drug Administration (FDA) and available to patients in Central Florida, giving hope that T1D will one day be completely curable.

“This is a significant breakthrough in the treatment of Type 1 diabetes,” shared Anna Casu, M.D., an investigator in T1D research at the AdventHealth Translational Research Institute and lives with Type 1 diabetes herself. “For the first time, a disease we thought was inevitable, can now be delayed.”
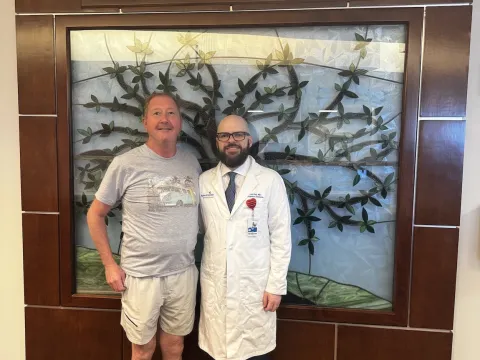
On Jan. 11, Konda Reddy, M.D., medical director of pediatric endocrinology and diabetes at AdventHealth for Children became the first in Central Florida and one of the first in the country to begin treating a patient with Tzield (teplizumab-mzwv). This is the first drug in the world to delay the onset of stage 3 T1D in adults and pediatric patients 8 years and older who currently have stage 2 T1D.

“Diabetes is a disease that never goes away, so delaying its onset can have a significant impact on quality of life for patients and their families,” said Dr. Reddy. “The approval of Tzield is a historic moment for the Type 1 diabetes community. It means there’s more time to live without the burden of the disease and its complications.”
An intravenous infusion delivered daily over the course of 14 days, Tzield is a CD3-directed monoclonal antibody treatment. It binds to CD3 antigens presented on the surface of T cells, delaying the onset of stage 3 T1D, when blood sugar levels are high, and symptoms typically begin.
Tzield’s safety and efficacy were evaluated in a randomized, double-blind, event-driven, placebo-controlled trial conducted by the Type 1 diabetes TrialNet (Trial Network) consortium. With over 200,000 participants screened globally since launch, AdventHealth served as one of the screening sites (U.S, Canada, and Europe) for TrialNet studies.
In the trial, 76 patients with stage 2 T1D randomly received Tzield or a placebo once daily via intravenous infusion for 14 days. Over a median follow-up period of 51 months, 45% of the 44 patients who received Tzield were later diagnosed with stage 3 T1D, compared to 72% of the 32 patients who received a placebo. The mid-range time from randomization to stage 3 T1D diagnosis was 50 months for the patients who received Tzield and 25 months for those who received a placebo.
According to the Juvenile Diabetes Research Foundation, approximately 1.45 million Americans are living with T1D, and 64,000 are diagnosed each year in the U.S. An autoimmune disease, T1D causes a person’s immune system to destroy insulin-producing cells, elevating blood glucose to dangerous levels. Those with T1D require daily insulin via injection or pump to survive.
Tzield is approved for people who are at high risk for T1D and have abnormal blood sugar levels determined by an oral glucose tolerance test. To meet the criteria for “high risk,” a person must have a screening test that confirms the presence of at least two specific autoantibodies that indicate the body is already attacking the insulin-producing beta cells in the pancreas.
To refer a pediatric patient for T1D screening or Tzield treatment, click here.
To learn more about diabetes research at the AdventHealth Translational Research Institute, click here.
Recent News

AdventHealth Cancer Institute Advances the Use of CAR T-Cell Therapy for Multiple Myeloma
CAR-T therapies have emerged as new treatment options for certain types of cancer through a one-time infusion that can lead to long-lasting remission.

New Clinical Trial Explores Digital Intervention for Apathy in Late-life Depression
Afflicting 30-50% of patients with late-life depression, apathy is a challenging psychiatric syndrome in older adulthood that can result in lack of motivation leading to poor self-care, physical...
AdventHealth Performs Central Florida’s First Liver Transplant for Unresectable Colorectal Liver Metastases
In June 2025, AdventHealth Abdominal Transplant Surgeon and Surgical Oncologist Ryan Day, MD, worked with a multidisciplinary team to perform Central Florida’s first liver transplant for unresectable...

AdventHealth Neuroscience Institute First in Florida to be Recognized as a GammaTile Center of Excellence
GammaTile is the first and only tile-based radiation therapy for the treatment of
operable brain tumors. The AdventHealth Neuroscience Institute began performing GammaTile procedures in 2021 and was...

An AdventHealth Collaboration Explores the Impact of Microgravity and Electrical Stimulation on Muscle Cell Health in Space
Using a muscle lab-on-chip model aboard the International Space Station (ISS), AdventHealth Translational Research Institute’s Dr. Paul Coen has been working with a multidisciplinary team from the...

AdventHealth Neuroscience Institute Among First in U.S. to Offer Phase IIa Clinical Trial of Troculeucel for Moderate Alzheimer’s Disease
While most clinical trials for Alzheimer’s disease have focused on patients with early or mild cognitive impairment, roughly 30% of those with Alzheimer’s have moderate stage disease for which there...

AdventHealth Translational Research Institute Selected as Clinical Site for National Study of Muscle, Mobility and Aging (SOMMA)
Under the leadership of Scientific Director and Principal Investigator Bret H. Goodpaster, PhD, the AdventHealth Translational Research Institute (TRI) is now enrolling men and women 70 years of age...

AdventHealth Neuroscience Institute Administers First Dose of Investigative NK Cell Therapy to Person with Alzheimer’s Disease
Under a single compassionate use Investigational New Drug (IND) authorization cleared by the U.S. Food and Drug Administration (FDA), the AdventHealth Neuroscience Institute worked with NKGen Biotech...

AdventHealth Study Exploring the Use of MR-Guided Focused Ultrasound (MRgFUS) to Disrupt the Blood-Brain Barrier for Treatment of Alzheimer’s Disease
Under the leadership of Dr. Valeria Baldivieso and Dr. Chandan Reddy, the AdventHealth Research Institute is the first and only site in Orlando offering the Exablate Blood-Brain Barrier (BBB)...

AdventHealth Research Institute Offers Phase II Clinical Trial of Etanercept for Treatment of Blast-Induced Tinnitus
Approximately 1 billion people throughout the world suffer from tinnitus (ringing in the ears), and it is the number one disability of those who serve in the U.S. military. The condition can disrupt...

AdventHealth Research Institute and NESTRE Health & Performance Announce Collaboration to Advance Neurocognitive Health and Performance Through Cognitive Training
With an aging population and increases in the prevalence of neurological conditions like Alzheimer’s disease and dementia, physicians and patients alike continue to seek new tools and approaches to...

AdventHealth Among First in U.S. to Offer IDP023-2-101 Clinical Trial for Patients with Progressive Multiple Sclerosis
The AdventHealth Neuroscience Institute is the first in Florida and one of the first in the country to begin recruiting patients with primary progressive or non-active secondary progressive multiple...
